Sacral plexus
The sacral plexus provides motor and sensory innervation to the gluteal region, many pelvic structures, and the posterior thigh, leg, and foot. It contains quite a few nerves that arise from the L4 and L5, and S1 to S4 vertebral levels.
The sacral plexus is a tangle of nerves that are related to the sacrum, thus the name. They weave together, intertwine, and work to provide motor and sensory innervation to organs in the pelvis, gluteal region, and posterior thigh and leg. There are some key ideas to keep in mind that'll help sort out the sacral plexus - let's get at 'em!
Plexuses in the abdomen and pelvis
While this post is about the sacral plexus in detail, we have to begin our discussion with a brief review of the nerves in the lumbar region, too.
The lumbar plexus is made of the ventral primary rami of spinal nerves from T12 and L1 to L5. Nerves that come from the lumbar plexus innervate structures in the leg and pelvis. This plexus deserves its own post so to get back to the sacral plexus here, let's quickly mention the named nerves from the lumbar plexus:
subcostal (T12)
iliohypogastric (L1)
ilioinguinal (L1)
genitofemoral (L1-2)
lateral femoral cutaneous (L2-3)
femoral (L2-4)
obturator (L2-4)
The nerves listed above are important, they just aren't part of the sacral plexus so we'll save them for their own post.
The nerve roots from L4 and L5 also form a structure called the lumbosacral trunk - this is how L4 and 5 fibers end up in the sacral plexus. In addition to the large lumbosacral trunk from L4-5, the sacral plexus also consists of S1-4 ventral primary rami. S1-4 exit the sacrum through the anterior sacral foramina. Most of the sacral plexus therefore lies on the posterolateral wall of the pelvis, with proximal branches lying on top of the piriformis muscle.
While the sacral plexus is formed from ventral primary rami of spinal nerves (the dorsal primary rami go into the back, instead), once the VPR get into the plexus they split into anterior and posterior divisions that correspond to the developmental progress of the muscular and cutaneous targets (anterior vs posterior orientation during embryological development).
Some branches of the sacral plexus stay in the pelvis while others exit to reach targets in the gluteal region, posterior thigh, knee, leg, and foot. Let's discuss each named nerve in turn, then we'll review the sensory and autonomic fibers associated with the sacral plexus.
Pelvic and gluteal branches of the sacral plexus
Muscles that form the pelvic floor, or the pelvic diaphragm, include levator ani (and its subparts) and the coccygeus muscles. These muscles form an important function by supporting pelvic organs and their passageway to the external world.
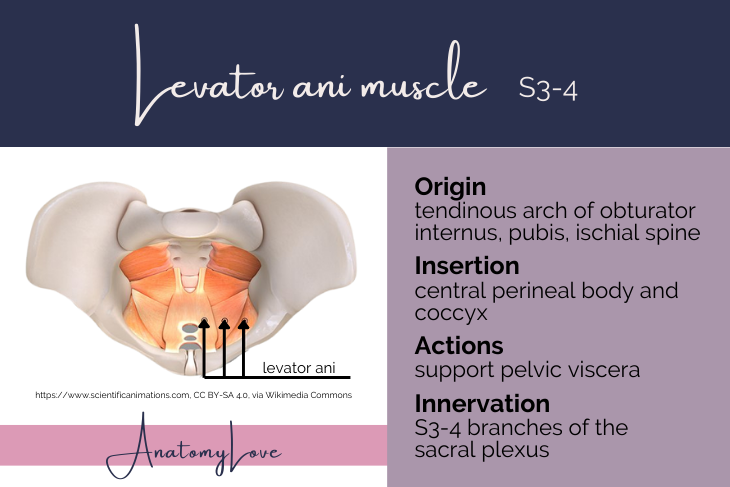
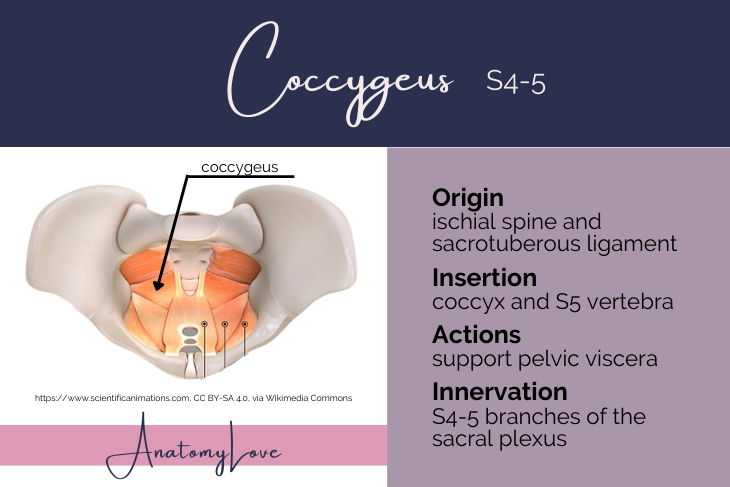
Levator ani and coccygeus muscles
Levator ani muscle originates from the tendinous arch of the obturator internus muscle and converges towards the midline to insert on the central tendon or perineal body, the external anal sphincter, the anococcygeal raphe, and the coccyx itself. Innervation to the levator ani muscle comes from S3-4 branches of the sacral plexus.
Together with levator ani, the coccygeus muscle completes the pelvic diaphragm. Coccygeus originates from the ischial spine and sacrospinous ligament. It inserts onto the coccyx and lateral margins of S5 vertebra. Innervation to the coccygeus muscles comes from S4-5 branches of the sacral (and coccygeal) plexus.
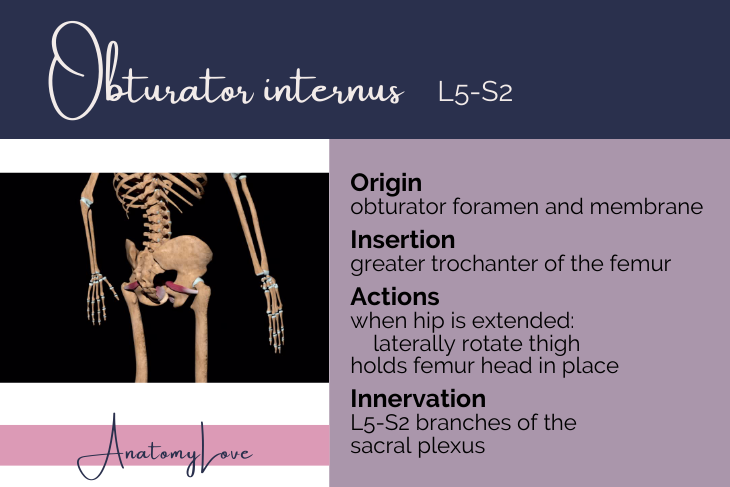
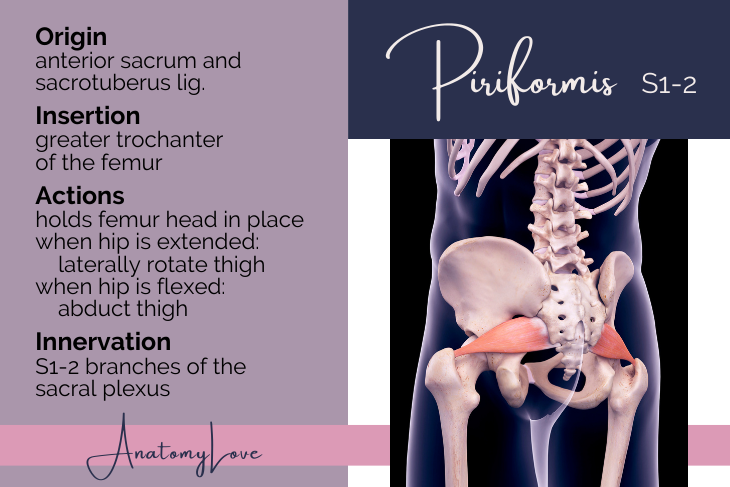
Obturator internus and piriformis muscles
The obturator internus muscle is innervated by L5-S2. From its origin on the internal aspect of the obturator membrane, the muscle condenses down to a tendon that exits the pelvis through the lesser sciatic foramen to insert onto the greater trochanter of the femur. The nerve to obturator internus does the same, innervating that muscle plus the superior gemellus muscle.
Piriformis muscle is a pear-shaped muscle innervated by S1-S2 nerves. It is easily found within the pelvis because it forms a bed on which the sacral plexus lies within the true pelvic cavity. In the gluteal region it is a good landmark because superior gluteal vessels and nerves exit the pelvis above it while the inferior gluteal neurovascular bundle, as well as the sciatic nerve, can be found below the piriformis muscle.
When the hip is extended the piriformis and obturator internus muscles laterally rotate the thigh. When the hip is flexed the piriformis abducts the thigh. Both also assist in holding the head of the femur in acetabulum of the os coxa.
External genital branches via pudendal nerve
Another branch of the sacral plexus is the pudendal nerve from S2-4. This one exits the pelvis through the greater sciatic foramen but quickly dives back into the perineum through the lesser sciatic foramen. It gives off inferior rectal nerves to the lower rectum, external anal sphincter, and adjacent skin. Then, the pudendal nerve branches into a dorsal nerve of the clitoris or penis and a perineal branch. Superficial and deep branches of the perineal nerve then innervate skin and external genital tissues.
Gluteal muscles
The superior gluteal nerve forms from L4-S1 portions of the sacral plexus. It exits the pelvis through the greater sciatic foramen, superior to the piriformis muscle. The superior gluteal nerve provides motor innervation to most gluteal muscles (gluteus medius, gluteus minimus, and tensor fascia lata). Notably, superior does not supply the gluteus maximum - that is the job of inferior gluteal nerve.
The inferior gluteal nerve forms from L5-S2, emerges from the pelvis through the greater sciatic foramen but inferior to the piriformis muscle, and innervates the gluteus maximum muscle.
Autonomic nerves
The rest of sacral plexus that stays in the pelvis serves autonomic functions there. Of note, the S2-4 levels have pre-ganglionic parasympathetic fibers known as pelvic splanchnic nerves (splanchnic means "visceral"). These synapse on neurons located in the walls of the target organs - the bladder, internal reproductive organs, erectile tissues, the descending and sigmoid colon, and the rectum. Visceral pain fibers also travel in the pelvic splanchnic nerves. (Note, don't confuse pelvic splanchnic nerves from the sacral plexus with sacral splanchnic nerves - those are post-ganglionic fibers from the sympathetic chain to the same targets. While they are autonomic fibers in the pelvis, they are not branches of the sacral plexus).
Sciatic nerve
The sciatic nerve is the largest nerve in the body - like as big as your thumb big - wowza! And it is long, too! It starts at the sacrum and branches from it go all the way to the foot. Crazy!
Many spinal levels contribute to the sciatic nerve - anterior divisions of L4 through S3, in fact. Sciatic nerve is mixed, meaning it contains motor and sensory fibers. The motor fibers run muscles in the posterior thigh on down to the foot (through its terminal branches). Sensory innervation from sciatic nerve is to the skin of the calf via a medial sural cutaneous nerve.
The course of the sciatic nerve is important (of course!). The many contributions to the sciatic nerve converge to exit the pelvis together through the greater sciatic foramen. Most of the time it then passes inferior to the piriformis muscle. In a small percentage of people though, all or part of the sciatic nerve passes through the piriformis muscle. This variation is called "piriformis syndrome" because of the nerve entrapment related to that muscle. It leads to pain that radiates down the posterior leg.
The sciatic nerve terminates in the popliteal fossa by dividing into two large nerves to the lower leg and foot. The common fibular branch of the sciatic nerve carries L4-S2 fibers while the tibial division carries L4-S3. Let's look at branches of those, too.
Tibial division of sciatic nerve
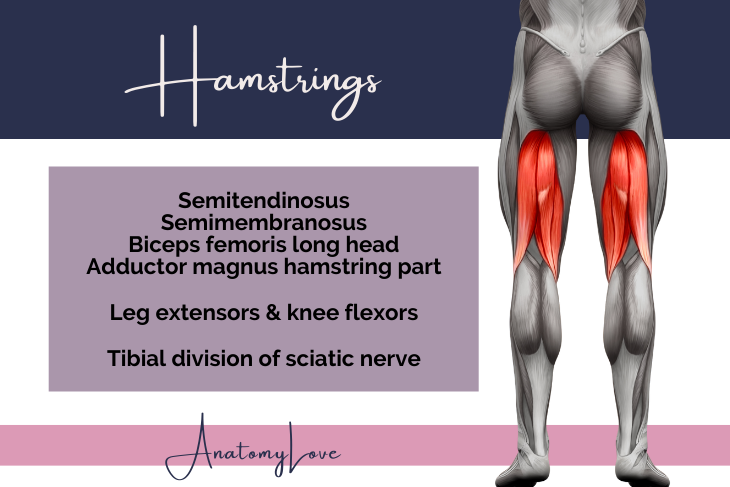
The tibial branch of the sciatic nerve includes muscular branches to muscles in the posterior compartment of the thigh - the hamstrings (semimembranosus, semitendinosus, and the long head of biceps femoris) and part of adductor magnus muscles. These muscles are extensors of the leg and flexors of the knee.
The tibial nerve goes on to innervate the gastrocnemius, soleus, popliteus, plantaris, and tibialis posterior muscles of the knee and calf. A sensory branch, the medial sural cutaneous nerve, innervates the skin of the calf. It terminates as the medial and lateral plantar nerves to muscles of the plantar foot.
Common fibular division of sciatic nerve
The common fibular branch of the sciatic nerve heads towards the lateral aspect of the lower leg. It divides into superficial and deep branches. While still in the thigh it innervates the short head of biceps femoris. In the leg it innervates muscles of the anterior and lateral compartments of the lower leg (tibialis anterior, extensor hallucis longus, extensor digitorum longus, and all three fibularis muscles through the superficial and deep branches), the extensor digitorum brevis on the dorsum of the foot, and then provides sensory innervation to the lateral leg and dorsum of the foot.
Cutaneous nerves from the sacral plexus
Most of the sensory cutaneous innervation that derives from the sacral plexus targets skin of the posterior thigh, knee, posterior leg, and both the plantar and dorsum of the foot.
Just so we cover the whole posterior lower limb, the middle cluneal (from the DPR of S1-3) and inferior cluneal (from posterior femoral cutaneous) nerves innervate skin over the buttocks. Note that the superior cluneal nerve also innervates skin of the gluteal region but arises from the lumbar plexus L1-3.
From the sacral plexus itself, the posterior femoral cutaneous nerve (S1-3) innervates skin of the lower buttocks region, the thigh, popliteal fossa, and even the proximal calf.
In the popliteal fossa both the tibial and common fibular divisions send branches that contribute to sensory innervation of the lower leg. The lateral sural cutaneous nerve comes from the common fibular nerve and moves towards the lateral lower leg. It usually has a communicating branch that joins the medial sural cutaneous nerve (from tibial nerve) to form the sural nerve.
Speaking of, the medial sural cutaneous nerve is a branch of the tibial nerve that comes off in the popliteal fossa. It forms the sural nerve of the calf when it is joined by a communicating branch of the lateral sural cutaneous (or directly from the common fibular) nerve. The target is skin of the posterior leg, along with the lateral portion of the ankle, heel, and foot.
The sural nerve is right in the middle of the posterior calf and is formed by the medial sural cutaneous nerve and a branch of the lateral sural cutaneous or a communicating branch from that same nerve. It runs with the lesser saphenous vein which is a good landmark for finding the nerve. Both of these structures lie right between the two heads of the gastrocnemius muscle so its cutaneous targets are the posterior leg, the lateral ankle, heel, and the foot.
Superficial fibular nerve is a branch of the common fibular nerve. It includes motor targets in the lateral compartment of the lower leg, but the skin it targets is the lateral side of the leg and the dorsum of the foot. Branches of this nerve include the medial dorsal cutaneous nerve to the medial foot and ankle, medial big toe, and skin of the second and third digits. An intermediate dorsal cutaneous nerve targets the skin of the lateral foot, ankle, and digits 3-5.
Deep fibular nerve is the other main branch of common fibular nerve. It is mostly a motor nerve, however it has a small cutaneous innervation to the web space between digits 1 and 2 (anatomists love to tag this one on practicals!).
Summary of sacral plexus
I hope this review has helped to better understand the sacral plexus. It gets a lot less love than the brachial plexus to the upper limb, but now that we've seen all that it does for the lower limb, I hope you think it deserves just as much attention.
With roots from L4-5 and S1-4, these nerves provide motor and sensory innervation to much of the pelvis, as well as the gluteal region, posterior thigh, popliteal fossa, anterior and posterior lower leg, and dorsal and plantar structures in the foot. Branches of the sacral plexus play a role in sexual function (autonomic fibers) and mobility.