Anterior triangle of the neck
This region connects the head to the neck and thorax. It contains important structures for the maintenance of basic life functions: breathing, eating and drinking, speech production, blood supply and drainage to the head, and movement of the shoulder. It is organized into several sub-triangles, as well as a superficial/muscular plane and a deep/visceral plane.
This region connects the head to the neck and thorax. It contains important structures for the maintenance of basic life functions: breathing, eating and drinking, speech production, blood supply and drainage to the head, and movement of the shoulder. It is organized into several sub-triangles, as well as a superficial/muscular plane and a deep/visceral plane. There is a whole lot to unpack, so let's go!
Boundaries
As with any new region, let's start by defining where we are in the body...the boundaries of the anterior triangle of the neck are:
Anterior: median line of the neck
Posterior: anterior border of SCM
Superior: inferior border of the mandible
Apex: jugular notch
Roof: subcutaneous tissue + platysma m.
Floor: visceral neck – larynx, pharynx, thyroid gland
The sternocleidomastoid muscle (SCM) is a key landmark for the anterior triangle of the neck since it forms the posterior border of this region. You might know that the SCM also forms the anterior border of the posterior triangle of the neck - read about that in the post on Lateral cervical region (aka: posterior triangle of the neck). Because this muscle is important for the whole neck, let's quickly review the factoids for it now:
The sternocleidomastoid muscle has two heads - one that originates from the anterior aspect of the manubrium of the sternum, and one that originates from the superior aspect of the medial third of the clavicle.
This broad muscle inserts onto the mastoid process of the temporal bone, just behind the ear, and along the lateral half of the superior nuchal line of the occipital bone.
The SCM has two actions depending on whether the left and right sides fire together or independently. When one side contracts, the unilateral action of that muscle is to laterally flex the neck and to rotate the face toward the contralateral (opposite) side. Acting together, the bilateral action of the SCMs are to flex the neck through the anterior longitudinal muscle fibers, and extend the atlanto-occipital joint via posterior longitudinal fibers. Finally, since this muscle attaches to the sternum and clavicle, it also acts as an accessory muscle of respiration.
Motor innervation to the SCM comes from the spinal accessory nerve, cranial nerve 11. Additional pain and proprioceptive fibers from the cervical plexus, C2-3 VPR (ventral primary rami) also innervate the SCM.
Finally, note that the sternocleidomastoid muscle is not a content of either the posterior (lateral cervical) or anterior triangles of the neck - it forms borders of both those regions but is not within either one.
Subtriangles
Anatomists love defining triangles in the body. Grab three nearby structures and viola - a triangle! So, do not be surprised that we also love subdividing triangles so we can get super specific as to region and contents.
Four sub-triangles are defined within the larger anterior triangle of the neck. Key muscles to identify the subtriangles are the omohyoid muscles and the digastric muscles - both of these have two bellies.
The digastric muscle consists of an anterior belly right under the chin and a posterior belly tucked under the angle of the mandible. The omohyoid muscle has a superior belly and inferior belly. In both the digastric and the omohyoid, the two muscle bellies are connected by a tendon and anchored to nearby bones - hyoid bone in the case of the digastric, and clavicle in the case of the omohyoid. Note though, that the inferior belly of omohyoid subdivides the posterior (lateral cervical) triangle of the neck into a large occipital (superior) subtriangle and a small omoclavicular/subclavian/supraclavicular (inferior) subtriangle. We will use the superior belly of the omohyoid to subdivide the anterior triangle of the neck since that is anterior to the sternocleidomastoid muscle.
Submental subtriangle of the anterior neck
The submental triangle is unpaired, meaning there is just one - located right under the point of the chin, also called the mentum of the chin (thus the name of the triangle).
The borders of the submental subtriangle are:
Lateral sides: L & R anterior digastric bellies
Base: hyoid bone
Apex: mentum and mandibular symphysis
Contents of the submental triangle are small submental lymph nodes and small veins that drain into the anterior jugular vein.
Submandibular (or digastric) subtriangle of the anterior neck
The submandibular subtriangle is named either for the main content here, the submandibular salivary gland, or the muscles that form it's borders, the digastric bellies. Think of this region as just under the inferior border and angle of the mandible but above the hyoid bone. There are two submandibular (digastric) subtriangles, one on each side. The borders are:
Lateral sides: anterior and posterior bellies of digastric m.
Base: inferior border and angle of mandible
Apex: digastric sling from hyoid bone
As the name implies, the main content of this subtriangle is the submandibular salivary gland, submandibular lymph nodes, the hypoglossal nerve (cranial nerve 12), the nerve to mylohyoid, and portions of the facial artery and vein (note that the submental vessels branch from/return to facial vessels in this subtriangle, though their targets are largely in the submental subtriangle).
Carotid subtriangle of the anterior neck
This clinically important subtriangle contains quite a bit for being pretty small. First, let's get solid on the borders of the carotid subtriangles, one on each side.
Posterior (base): anterior border of SCM
Anterosuperior: posterior belly of digastric
Anteroinferior: superior belly of omohyoid
The carotid triangle takes it's name from the very important contents that run through it:
Carotid sheath contents: carotid arteries (internal and external, along with proximal branches of the external carotid artery), the internal jugular vein, and the vagus nerve (cranial nerve 10)
Also in this subtriangle but NOT in the carotid sheath, the hypoglossal nerve (cranial nerve 12)
It is worth quickly emphasizing the contents of the carotid sheath: the carotid arteries, internal jugular vein (IJV), and the vagus nerve (cranial nerve 10). The arteries are located more medial/deep in the sheath, the IJV is lateral in sheath, and the vagus nerve is nestled between/posterior to the vasculature.
Also of note here, a loop of nerves, the ansa cervicalis, lies on anterolateral aspect of carotid sheath (but not in it). We'll review more of these nerves below.
Also of note in this subtriangle is the fact that the common carotid arteries bifurcate into internal and external branches at the C4 vertebral level which corresponds to the superior border of thyroid cartilage, for palpation purposes.
Speaking of palpation - the carotid arteries are quite large and this a one place to take a pulse in the neck. Careful not to push too hard though, as the carotid sinus (a dilation of the internal carotid artery just superior to it's bifurcation from the common carotid artery) and the carotid body (neural tissue nestled into the carotid bifurcation) are important visceral afferent monitors found at this level. The carotid sinus is a baroreceptor sensing blood pressure in the carotid vessel while the carotid body is a chemoreceptor that monitors oxygen and carbon dioxide levels in the blood. Both of these innervations are SVA (special visceral afferent) fibers that are carried by cranial nerve 9 (glossopharyngeal nerve) with a little help from cranial nerve 10 (vagus nerve). Low blood pressure and/or oxygen levels initiate a reflex to increase respiratory rate and heart rate.
Muscular subtriangle of the anterior neck
Compared to the carotid subtriangle, the muscular subtriangle is pretty straight forward. The borders are:
Anterior: median plane of the neck
Posterosuperior: superior belly of omohyoid
Posteroinferior: anterior border of SCM
The muscular subtriangle contains a group of strap-like muscles known as the infrayhoids because they are inferior to the hyoid bone. We'll cover them in more detail below. Also in this triangle are the thyroid and parathyroid glands and the trachea. The thyroid cartilage is palpable, as is the cricoid cartilage just inferior to it. Superficial and deep lymph nodes of the neck also lie in this region.
Fascia related to the anterior neck
Fascia of the cervical region are many and multilayered. Since we're working on the anterior triangle of the neck here, pertinent fascial layers include - from superficial to deep:
Superficial fascia (fat and cutaneous neurovascular bundles, and notably the absence of the platysma muscle which really covers the lateral cervical region and the sternocleidomastoid muscle, but is absent over the anterior triangle)
(Technically a thin sheet of investing layer of deep cervical fascia would be next, connecting left and right sternocleidomastoid muscles since that fascia surrounds that muscle)
Muscular portion of pretracheal deep cervical fascia - this is where the strap muscles of the neck are found
Visceral layer of pretracheal deep cervical fascia, containing the thyroid and parathyroid glands, the trachea, and the esophagus
(Technically, a thin sheet of fascia known as the alar fascia would be next, connecting the left and right carotid sheaths. But by now we are out of the "anterior triangle of neck" and into the retropharyngeal space, just anterior to the prevertebral layer of deep cervical fascia).
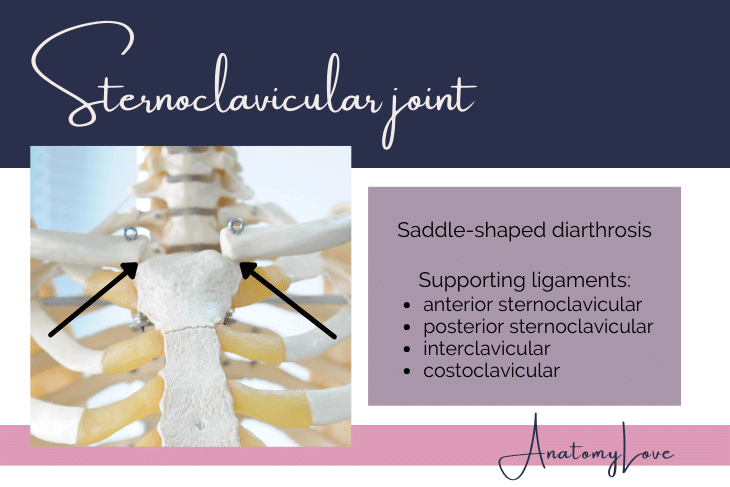
Sternoclavicular joint
The sternoclavicular joint is a saddle-shaped diarthrodial joint between the concave clavicular notch of the sternum and convex medial (sternal) end of the clavicle. Though synovial, the joint is lined by fibrocartilage and divided into two compartments by a fibrocartilage articular disc anchored to the joint capsule, clavicle, and first costal cartilage. The joint is located at the T1 vertebral level.
Blood supply to the sternoclavicular joint comes from the internal thoracic and suprascapular arteries. It is innervated by medial supraclavicular nerves and the nerve to subclavius.
Several strong ligaments support this joint. Anterior and posterior sternoclavicular ligaments surround it. The interclavicular ligament connects sternal ends of the left and right clavicle. A strong costoclavicular ligament anchors the medial clavicle to the costal cartilage of rib 1.
The subclavius muscle braces the clavicle as the arm moves, further supporting the sternoclavicular joint. Additionally, the anterior surface of the joint and ligaments is covered by the origin of the sternocleidomastoid muscle. The posterior side is covered by the origins of sternohyoid and sternothyroid muscles. The venous angle and brachiocephalic veins form just posterior to the joint. All these muscular and ligamentous relationships make the sternoclavicular joint very strong. The clavicle is likely to fracture before the sternoclavicular joint dislocates.
The axis of movement for the sternoclavicular joint is through the costoclavicular ligament. Protraction and retraction of scapula on thorax, and elevation and depression of the scapula are possible. Circumduction happens through coordination with the pectoral girdle and glenohumeral joint.
Hyoid bone
The hyoid bone is an excellent landmark in the anterior neck. It is readily palpable at the C3 vertebral level. It sub-divides the anterior cervical region into suprahyoid and infrahyoid muscle groups (discussed below). It is a free-floating bone with no other bony attachments - it is held in place by ligaments and muscles. Those structures connect the hyoid bone to the mandible, styloid process, thyroid cartilage, manubrium, and scapulae. The larynx is suspended inferiorly from the hyoid bone by the thyrohyoid membrane.
Cartilages of the anterior neck
The visceral layer of the anterior triangle includes two palpable cartilages that serve as attachments for muscles and protect the larynx. They are the thyroid and cricoid cartilages.
Thyroid cartilage
The thyroid cartilage protects the larynx and vocal cords. It is rather tall, running from the C4 to C5 vertebral levels. It serves as a good landmark for these levels and other structures in the neck. The thyroid cartilage is suspended from the hyoid bone by the thyrohyoid membrane.
The thyroid cartilage is shaped like a shield. Two continuous lamina face anteriorly while the posterior aspect is open. Superior and inferior horns (also known as cornu) project from the posterior borders. A large notch in the superior border is commonly known as the "adam's apple" or more technically, the laryngeal prominence. The oblique line on the anterolateral surface marks the place of muscle attachments for the sternothyroid, thyrohyoid, and inferior constrictor muscles.
Cricoid cartilage
The cricoid cartilage is a full ring of cartilage that lies at the C6 vertebral level. It is suspended from the thyroid cartilage by the cricothyroid membrane/ligament (site of “trach tubes”). The cricoid cartilage protects the infraglottic space of the larynx. The trachea begins just inferior to it.
Nerves of the anterior triangle of the neck
Just like the posterior triangle (lateral cervical region) of the neck, the anterior triangle is packed with nerves, including spinal nerves, cranial nerves, and autonomic nerves. Let's break them down piece by piece.
Cervical plexus
The cervical plexus is formed from the ventral primary rami of C1-C4. One interesting feature of the cervical plexus VPR (ventral primary rami) is that they are connected by loops of nerves - this doesn't happen in the brachial plexus lower in the neck. Several of the nerves discussed below are formed from two or more nerve roots by using these loops connecting VPR.
The cervical plexus of nerves came up in the post on the lateral cervical region (posterior triangle of the neck) because it includes sensory/afferent cutaneous fibers from Erb's point, or the nerve point of the neck. One of those branches, the transverse cervical nerve from C2-3 VPR crosses anterior to the sternocleidomastoid muscle to provide sensory innervation to the skin of the anterior triangle. Also from Erb's point are nerves from C2-3 that provide pain and proprioception innervation from the sternocleidomastoid muscle and similar nerves from C3-4 that do the same for the trapezius muscle. See the post on the lateral cervical region linked previously for more information on the rest of the sensory component of the cervical plexus.
Of note in the anterior triangle, related to the Erb's point sensory component of the cervical plexus, are C1 nerves that have a peculiar relationship with the hypoglossal nerve (cranial nerve 12). These fibers use the hypoglossal nerve to hitchhike their way to their targets. These hitchhikers include:
descendens hypoglossi nerve (superior root of ansa cervicalis n., discussed below)
nerve to thyrohyoid (to the thyrohyoid muscle)
nerve to geniohyoid muscle
Ansa cervicalis
Ansa cervicalis is a loop of nerves that arise from the ventral primary rami (VPR) of C1-3 spinal nerves. The loop of nerves provides motor innervation to most of the infrahyoid "strap" muscles of the anterior triangle. Of note, it is found lying on the lateral side of the internal jugular vein but not within the carotid sheath.
Phrenic nerve
An important nerve in the anterior triangle is the phrenic nerve. Technically it is a branch of both the cervical and brachial plexuses of nerves since it comes from the VPR (ventral primary rami) of C3, 4, and 5. It runs from those roots straight inferiorly along the anterior surface of the anterior scalene muscle (a great landmark in the lower neck!). Sometimes a small accessory phrenic nerve courses along with the main phrenic nerve. Always, a small artery, the ascending cervical artery, courses medial and parallel to the phrenic nerve. From the root of the neck, the phrenic nerve enters the superior thoracic aperture to course along the pericardium towards the diaphragm. Very importantly, the phrenic nerve provides motor innervation to the diaphragm which is why upper cervical injuries can be so dangerous. Severance would paralyze the ipsilateral side.
Cranial nerves in the anterior triangle of the neck
Now let's run through some of the cranial nerve branches that course through the anterior triangle. The ones that pop up will be a small nerve from the trigeminal nerve (cranial nerve 5), the glossopharyngeal nerve (cranial nerve 9), the vagus nerve (cranial nerve 10), and the hypoglossal nerve (cranial nerve 12). Remember that the spinal accessory nerve (cranial nerve 11) is found in the neck but it runs through the posterior triangle (lateral cervical region) of the neck since it's targets are the sternocleidomastoid and trapezius muscles.
Mandibular division of the trigeminal nerve
The trigeminal nerve has three divisions and the one that sends a branch to the anterior triangle of the neck is the mandibular division, also known as cranial nerve V3 (the third division). One small motor nerve that runs through the submandibular and submental subtriangles is the nerve to mylohyoid, providing motor innervation to the mylohyoid and anterior digastric muscles. Of note, this nerve runs superficial to mylohyoid m., whereas most muscles receive motor innervation from their deep sides.
Glossopharyngeal nerve
Glossopharyngeal nerve, cranial nerve 9, provides visceral afferent/sensory innervation from the carotid body and sinus located at the origin of the internal carotid artery. See that section above for more information about those nerves.
Of note for here and the rest of the neck, much of what the glossopharyngeal nerve does is also done by the vagus nerve, cranial nerve 10 because they contribute to the messy plexus of nerves known as the pharyngeal plexus. While most of the afferent fibers from the carotid body and sinus run in the glossopharyngeal nerve, some also course within the vagus, too.
Vagus nerve
The vagus nerve, cranial nerve 10, is a rock star in the neck and beyond! It courses out of the jugular foramen (along with cranial nerves 9, 10, and 11) and runs into the carotid sheath. High up in the neck a large branch moves medially towards the larynx. The superior laryngeal nerve has two branches itself - an internal branch that goes into the larynx to provide sensory innervation to the mucosa of the upper larynx, and a very small external branch that stays outside of the larynx to provide motor innervation to the cricothyroid muscle, a laryngeal muscle that technically lies in the anterior triangle of the neck between the thyroid and cricoid cartilages.
Another large and important branch of the vagus nerve, the recurrent laryngeal nerve, is found in the root of the neck. There is asymmetry in how this nerves forms. On the right side the recurrent laryngeal nerve forms and loops around the right subclavian artery. However, on the left side, the recurrent laryngeal nerve doesn't loop back up into the neck until the vagus reaches the arch of the aorta. Both recurrent laryngeal nerves move into the larynx where they provide sensory innervation to the lower larynx and motor innervation to all laryngeal muscles.
It is important to remember that the vagus nerve is the main parasympathetic and sensory nerve below the neck, serving viscera of the thorax and most of the abdomen. Thus, it continues inferiorly after the recurrent laryngeal nerves branch off.
Hypoglossal nerve
The hypoglossal nerve, or cranial nerve 12, is a large nerve that exits the hypoglossal canal of the occipital bone to course around and run transversely through the submandibular triangle of the neck. The job of the hypoglossal nerve is to provide motor innervation to muscles with "-glossal" in their name, so tongue muscles (except for palatoglossus muscle, whose motor innervation comes from the vagus nerve).
The hypoglossal nerve follows the inferior border of the posterior belly of the digastric muscle then passes between the external carotid artery and internal jugular vein, then shoots between the mylohyoid and hyoglossus muscles to finally reach base of the tongue.
The hypoglossal nerve carries C1 hitchhikers along the way (nerve to thyrohyoid, geniohyoid nerve, and the superior root of the ansa cervicalis).
Sympathetic chain in the cervical region
Deep within the anterior triangle of the neck, nearly embedded in the prevertebral layer of deep cervical fascia, is the cervical sympathetic chain and three cervical sympathetic ganglia. Sympathetic nerves are part of the autonomic nervous system - they provide the "fight or flight" response that increases heart rate, respiratory rate, and shunts blood to skeletal muscles.
Anatomically, it is important to know that the sympathetic chain runs medial to the carotid sheath, not inside it.
There are three ganglia on the sympathetic chain in the cervical region:
Superior cervical ganglion lies at the C1-3 vertebral levels (it is big!) and sends gray rami communicantes into the VPR of C1-4 spinal nerves.
Middle cervical ganglion lies at the C6 vertebral level and sends gray rami communicantes into the VPR of C5-6 spinal nerves.
Inferior cervical ganglion lies at the C7 vertebral level and sends gray rami communicantes into the VPR of C7-8 spinal nerves.
Technically in the thorax, let's also mention the stellate (cervicothoracic) ganglion that sits at the T1 vertebral level and sends it's gray rami communicantes into the T1 spinal nerve.
Autonomic innervation is quite important, as you might imagine. It gets it's own post. But for now, know that there are no white rami communicantes in the neck (they only exist as high as the T1 spinal nerve). All rami communicantes in the neck are the post-ganglionic, unmyelinated fibers mentioned above, gray rami communicantes, carrying sympathetic fibers into the periphery through spinal nerves and embedded within the tunica adventitia (outer layer) of blood vessels.
There is a thin loop of nerves that connects the middle and inferior cervical sympathetic ganglia, a collateral route besides the sympathetic chain itself, known as the ansa subclavia ("ansa" means handle, or loop).
Another notable sympathetic nerve in the cervical region is the carotid nerve, an extension of the post-ganglionic sympathetic fibers leaving the chain superiorly, following the internal carotid artery into the cranial cavity. Similar fibers follow the external carotid artery though they are never quite as big as the ones accompanying the internal carotid artery into the carotid canal so they don't get their own name.
Finally, in addition to the gray rami communicantes connections with spinal nerves mentioned above, all three sympathetic ganglia send gray rami medially into the pharyngeal plexus of nerves (recall that cranial nerves 9 and 10 also do this). These nerves are known as the cardiopulmonary plexus since they are using the pharyngeal fascia to course inferiorly towards thoracic viscera.
Muscles of the anterior triangle of the neck
Muscles in the anterior triangle of the neck support the hyoid bone and form the floor of the oral cavity. The hyoid bone is used to divide anterior triangle muscles into "suprahyoid" (above the hyoid bone) and "infrahyoid" (below the hyoid bone) groups of muscles.
Suprahyoid muscles
Suprahyoid muscles are found above the hyoid bone and connect it to the skull and mandible (recall that the hyoid has no bony articulations, only muscles and ligaments that hold it in place).
Suprahyoid muscles form the floor of the submandibular and submental subtriangles, and thus also the floor of the mouth. They act to elevate and retract the hyoid bone and larynx when swallowing and speaking.
There are several suprahyoid muscles:
Mylohyoid - from the mylohyoid line of the inside/deep aspect of the body of the mandible to the hyoid bone, forming the floor of the oral cavity and submental triangles. This muscle is innervated by the nerve to mylohyoid from the mandibular division of the trigeminal nerve.
Geniohyoid - from the inferior genial/mental spine near the midline inside/deep aspect of the mandible to the hyoid bone. This muscle is innervated by a fiber from the C1 VPR that gets there by hitchhiking on the hypoglossal nerve.
Stylohyoid - originates from the styloid process of the temporal bone and inserts onto the hyoid bone, helping to elevate and retract the hyoid like the rest of the suprahyoid muscles. This muscle is innervated by the facial nerve, cranial nerve 7.
Digastric - this muscle has two bellies, a posterior and anterior portion connected by an intermediate tendon anchored to the hyoid bone by fascia. The posterior belly of the digastric muscle originates on the inside aspect of the mastoid process of the temporal bone while the anterior belly of digastric originates at the digastric fossa near the midline on the inside/deep side of the mandible. The posterior digastric muscle is innervated by the facial nerve while the anterior belly is innervated by the nerve to mylohyoid from the mandibular division of trigeminal nerve.
Infrahyoid muscles
The infrahyoid muscle group is by definition, below or inferior to the hyoid bone. These are often referred to as the "strap" muscles because of their long, thin, linear shape.
The infrahyoid muscles connect to the inferior aspect of the hyoid bone and superior border of sternum, and connect the hyoid bone to the clavicle and scapula. Their attachments allow them to anchor the hyoid and shoulder girdle, steady the hyoid bone, and depress it (and the larynx) during swallowing and speaking.
The infrahyoid muscles are found in two planes - superficial and deep. The superficial plane includes the sternohyoid muscle and the superior belly of the omohyoid muscle. The deep plane includes the sternothyroid and thyrohyoid muscles.
Sternohyoid - from the deep/internal surface of the manubrium of the sternum to the inferior aspect of the hyoid bone. Motor innervation to this muscle comes from ansa cervicalis, C1-3 VPR fibers from the cervical plexus.
Sternothyroid - from the deep/internal surface of the manubrium of the sternum to the inferior aspect of the oblique line of the thyroid cartilage. Motor innervation to this muscle comes from ansa cervicalis, C1-3 VPR fibers from the cervical plexus.
Thyrohyoid - from the oblique line of the thyroid cartilage to the inferior aspect of the hyoid bone. Unlike the rest of the "strap" muscles, thyrohyoid is innervated only by C1 VPR fibers that hitchhike with the hypoglossal nerve to get to that muscle (those fibers are often called the "nerve to thyrohyoid").
Omohyoid - this muscle has two bellies, a superior one that is within the anterior triangle of the neck (and an inferior one that forms subtriangles in the posterior triangle or lateral cervical region). The two bellies are connected by an intermediate tendon which is anchored to the clavicle. The inferior belly originates on the superior border of the scapula, just medial to the suprascapular notch, and inserts onto that intermediate tendon. The superior belly originates from that tendon to insert onto the hyoid bone. Motor innervation to both bellies comes from ansa cervicalis, C1-3 VPR fibers from the cervical plexus.
Arteries of the anterior triangle
One of the key concepts of the anterior triangle of the neck is the branching, course, and distribution of blood to the neck and head. Large arteries of the anterior triangle come from the common carotid arteries. To get there, let's quickly review branches of the arch of the aorta: brachiocephalic trunk, left common carotid artery, and the left subclavian artery. The brachiocephalic trunk branches into a right common carotid artery and right subclavian artery.
Of note in the anterior triangle are the common carotid arteries and their branches. The carotid arteries course within the carotid sheath (with the internal jugular vein and the vagus nerve). Around the C4 vertebral level (on par with the superior border of the thyroid cartilage) the common carotid arteries branch into internal and external carotid arteries. The carotid body and sinus mentioned above are found at this bifurcation and within the internal carotid artery itself.
Internal carotid artery
The internal carotid artery (ICA) actually has no branches in the neck so we'll only quickly mention it's position and neurological sensory components here. The internal carotid artery is so named because it enters the cranial cavity at the carotid canal of the petrous portion of the temporal bone and actually supplies the anterior and ventral aspects of the brain itself. It's position in the carotid sheath of the neck is towards the outside/lateral though, so don't let that confuse you. It is named for it's course, not position in the neck.
As mentioned above, the internal carotid artery includes a dilation near it's bifurcation from the common carotid artery, the carotid sinus. This area includes baroreceptors to sense blood pressure in this large vessel rather close to the heart. Also at the bifurcation is a little piece of neural tissue, the carotid body, which is a chemoreceptor sensing the concentration of blood gases like oxygen and carbon dioxide.
External carotid artery and branches
The external carotid artery (ECA) is named for it's distribution on the external side of the cranium (as opposed to the internal carotid artery which supplies a lot of the inside of the cranial cavity). It is within the carotid sheath, though deep to the internal carotid artery. Branches of the external carotid artery are many - they supply a whole lot so let's cover them below:
The first branch of the external carotid artery is superior thyroid artery which supplies:
Superior pole of thyroid gland
Thyrohyoid, SCM, and cricothyroid muscles
Superior laryngeal artery which supplies the supra-glottic larynx
Course: moves inferior, right after branching from ECA
The second branch of the external carotid artery is the ascending pharyngeal artery which supplies:
Pharyngeal constrictors & stylopharyngeus mm.
Soft palate, tonsils, auditory tube
Meningeal br. moves through jugular foramen to supply posterior cranial fossa meninges
Course: forms near bifurcation on medial side of ECA; runs directly superior from there
The third and a rather large branch of the external carotid artery is the lingual artery which supplies:
Muscles of the tongue, palatine tonsil, soft palate, epiglottis, floor of mouth, sublingual glands
Course: may form trunk with the facial a.; dives towards the base of the tongue behind (deep to) the hyoglossus m. near it’s origin from the hyoid bone
The fourth and also rather large branch of the external carotid artery is the facial artery and it supplies:
Superficial anterior face muscles, submandibular gland, soft palate and palatine tonsils, auditory tube
Course: forms near the angle of the mandible, runs deep to posterior belly of the digastric m., through the submandibular gland, to emerge onto the face at the inferior border of the mandible; runs obliquely towards the medial canthus of the eye
The fifth branch of the external carotid artery is the occipital artery which supplies:
Sternocleidomastoid m., meninges in posterior cranial fossa, mastoid air cells, deep back muscles, posterior scalp
Course: posterior br. that forms near or superior to the angle of the mandible, runs deep to posterior digastric m. towards the occipital groove on the medial mastoid process, then across posterior scalp
The sixth branch of the external carotid artery is a small posterior auricular artery which supplies:
External ear and scalp behind ear, parotid gland and muscles nearby, middle and inner ear structures
Course: posterior br. that forms near the tip of the mastoid process, then runs posterior-superior to the scalp behind the ear
The seventh branch of the external carotid artery, and one of the terminal branches of the ECA is the maxillary artery and it supplies, via three parts:
External acoustic meatus and tympanic membrane, TMJ, dura mater and diploe of lateral skull, ganglion of CN V (trigeminal n.) & nearby dura
Mandibular teeth and gums, all muscles of mastication including mylohyoid m., skin of the chin
Maxillary teeth and gums, maxillary sinus mucosa, skin and muscles in the infra-orbital region of the face, the soft palate and anterior portion of the hard palate, the roof of the nasopharynx, and the nasal cavity walls and septum
Course: largest of the 2 terminal ECA brs., it forms posterior to the neck of the mandible then courses through the infratemporal fossa to terminate in many branches within the pterygopalatine fossa
The eighth and other terminal branch of the ECA is the superficial temporal artery which supplies:
Parotid gland and duct, lateral superficial face, anterior part of external ear, masseter and temporalis mm., temporal fossa
Course: smaller of the 2 terminal ECA brs., runs superiorly from near the neck of the mandible, anterior to the ear, superficial to the zygomatic arch, to end in posterior and anterior branches
Internal jugular vein and tributaries
The internal jugular vein (IJV) is the largest vein in the neck - about the size of one of your fingers! The large size is due to the fact that it drains the brain, face, cervical viscera, and deep muscles of the neck.
The internal jugular vein forms at the jugular foramen. From there it runs within carotid sheath, lateral and superficial to the carotid vessels.
In the root of the neck the internal jugular vein meets the subclavian vein, just deep and a tad superior to the sternoclavicular joint. These two large veins form the right and left brachiocephalic veins at what is termed the venous angle. Lymphatic vessels empty back into the venous system at the venous angles (we'll cover lymphatics below). Along it's course, deep cervical lymph nodes run with the internal jugular vein.
The inferior section of the internal jugular vein is dilated and contains an internal valve to prevent blood flow back into neck and head (as when inverted; Trendelenburg position).
Of particular anatomical note, the ansa cervicalis nerves are found on the IJV, though external to the carotid sheath.
Tributaries to the internal jugular vein in the neck include:
Common facial vein formed by the facial vein, anterior division of retromandibular, and the lingual vein
Superior and middle thyroid veins
Occipital v. (sometimes, usually it would go to the suboccipital venous plexus)
Inferior petrosal sinus (a dural venous sinus)
Pharyngeal venous plexus
Clinical aspects of large neck vessels
With such large and important vessels in the anterior triangle and root of the neck, let's briefly review a few procedures and clinical aspects that utilize these vessels.
Catheterization and the internal jugular vein (ports take advantage of this same anatomy); right cardiac catheterization measures pressure in the right side of the heart. Access can be introduced through the inferior portion of the right internal jugular vein which quickly forms the right brachiocephalic vein then the superior vena cava (access could also be through subclavian vein).
Ligation of external carotid artery is used to control bleeding in the regions fed by this artery. Ligation of one slide slows blood flow, though blood from the other side anastomoses across the midline.
Surgeries within the carotid subtriangle may injure either the superior or recurrent laryngeal nerves, branches of cranial nerve ten the vagus nerve, and would affect sensory and motor capacities of the larynx.
Also in the carotid subtriangle, the carotid pulse is best felt along the common carotid artery between the trachea and the infrahyoid "strap" muscles just deep to the anterior border of the sternocleidomastoid muscle (avoid direct pressure of the carotid sinus)
Occlusion in the internal carotid artery may be due to atherosclerotic thickening of tunica intima, obstructing blood flow to the brain. Transient ischemic attack – focal loss of neurological function seen as dizziness and disorientation lasting ~24 hrs or minor stroke – same as above including weakness and sensory loss on one side lasting 1-21 days may occur. A Doppler color study to visualize (ultrasound) blood flow and/or occlusions may be necessary.
Lymphatics of the anterior neck
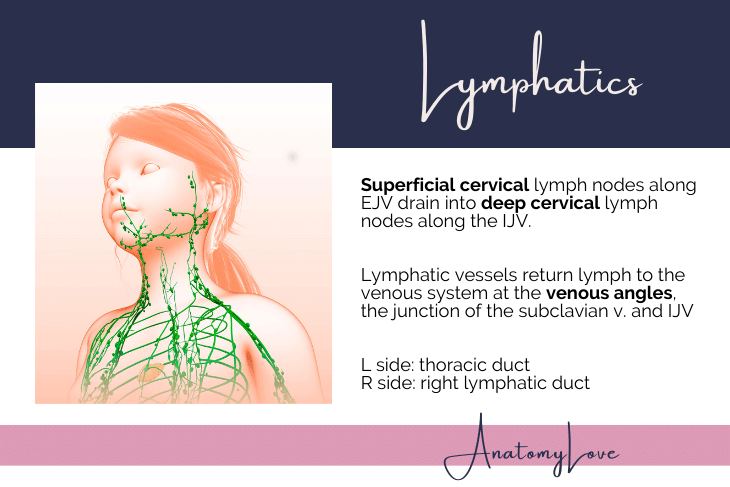
Lymph vessels collect excess interstitial fluid (lymph) for return to the venous system. Delicate tangles of lymph vessels course throughout the body and form ever-larger vessels that flow towards the root of the neck.
Generally speaking, superficial cervical lymph nodes are scattered along the external jugular vein and receive lymph from the skin and superficial fascia. Deep cervical lymph nodes are scattered along the internal jugular vein and receive lymph from the viscera and deep muscles of the neck and back.
Lymphatic vessel formation is not symmetrical. However, all lymph fluid returns to the venous system at the venous angles, the junction of the subclavian vein and internal jugular vein, in the root of the neck.
On the right side, lymph from the right arm, the right shoulder, right side of the neck and head, and upper thorax and breast ultimately drains into the right lymphatic duct at the right venous angle.
The left venous angle receives the thoracic duct, collecting lymph from everywhere else in the body.
Submandibular gland
The submandibular gland is a salivary gland that is tucked right under the inferior border of the mandible - thus the name! This gland is about the size of a walnut with one long duct that opens underneath the tongue at a little bump called the sublingual caruncle. You can see your own, too! Look under your tongue on either side of the lingual frenulum (that thin fold of mucosa that anchors your tongue to the floor of your mouth) - there is one pea-sized lump on either side - that is the sublingual caruncle. The submandibular duct opens up right there.
Fun fact! This is where "gleeking" happens...you know, when you inadvertently spray saliva a shockingly long distance across the room, usually while yawning or when it is embarrassing to do so. Some people can do this on command (I've never tried, myself!). Now you know, though!
Remember all those subtriangles mentioned above? The submandibular gland sits within the submandibular subtriangle because it is large enough that it occupies most of that space. Recall that the subtriangle is bounded by the posterior and anterior digastric muscle bellies so that subtriangle is sometimes called digastric, too.
Blood supply to the submandibular gland comes from the facial artery as it courses from the external carotid artery (in the carotid subtriangle) towards the face. The facial artery courses just deep to the submandibular gland, or sometimes even within it.
Salivary secretions from the submandibular gland come by way of the facial nerve, too (cranial nerve 7). These parasympathetic fibers originate from pre-ganglionic neurons located in the superior salivary nucleus in the pons. The nerve exits the brain stem with the rest of cranial nerve 7, moves into the internal auditory meatus and splits from the rest of the facial nerve (parts that will go on to innervate muscles of facial expression and most of the rest of the salivary glands in the head) to form the chorda tympani nerve. This small nerve exits the petrotympanic fissure on the base of the cranium, just under the ear and posterolateral to the foramen ovale. Chorda tympani nerve then joins a branch of the mandibular division of trigeminal, the lingual nerve, because it needs to get into the mouth. Since the parasympathetic fibers in chorda tympani are still pre-ganglionic, the relationship to the lingual nerve is important because the post-ganglionic neurons are located in the submandibular ganglion which dangles off of the lingual nerve as it enters the posterior aspect of the oral cavity. Once chorda tympani's nerve fibers synapse in the submandibular ganglion it is a short trip to innervate the sublingual and submandibular salivary glands in the oral cavity. Finally, note that special sensory/afferent fibers are also traveling in the chorda tympani nerve; these come from taste buds on the anterior two-thirds of the tongue.
Thyroid gland
The thyroid gland is an endocrine gland producing thyroid hormones T3 (triiodothyronine)and T4 (tetraiodothyronine), as well as calcitonin. Thyroid hormones have wide and pervasive effects in the body such as increasing base metabolic rate, increasing heart rate and force of contraction, as well as vasodilation. Calcitonin acts on bone cells and the kidney to help lower the concentration of calcium in the blood should it become too high.
Interestingly enough, the thyroid gland develops on the dorsum of the tongue at the foramen cecum, then migrates down through thyroglossal duct (cysts may persist along this route). Parathyroid glands (four total) are embedded in the posterior aspect of the thyroid gland.
Anatomically, the thyroid gland is found within the visceral layer of pretracheal fascia, covered somewhat by the infrahyoid "strap" muscles. Left and right lobes of the thyroid gland surround the trachea, connected by a midline isthmus at the C7 or T1 vertebral level. Aberrant, accessory, or pyramidal lobes of thyroid may be present.
Blood supply to all endocrine glands is pervasive, and for the thyroid gland it comes from two different sources:
Superior thyroid artery from the external carotid artery
Inferior thyroid artery from the thyrocervical trunk and subclavian artery
A thyroid ima artery may be present (~10%)
Venous return from the thyroid gland is to the superior, middle, inferior thyroid veins. The superior and middle thyroid veins empty into the internal jugular vein. The inferior thyroid vein empties into the left brachiocephalic vein.
Superior, middle, and inferior cervical sympathetic ganglia all send branches to the thyroid arteries to influence blood flow (vasomotor) to the gland. Sympathetics cause constriction of blood vessels (thyroid hormone is made from blood products so it would reduce blood flow and thyroid hormones).
Goiter is an enlarged thyroid gland due to lack of iodine in the blood. An enlargement of the thyroid gland could compress trachea, esophagus, recurrent laryngeal nerves which run close by. Expansion of the thyroid gland is limited in superior expansion by the infrahyoid "strap" muscle attachments on the thyroid cartilage and hyoid bone so an enlarged thyroid gland is usually seen and felt lower in the neck.
Hyperthyroidism is an overactive thyroid gland, which increases metabolism too much leading to noticeable weight loss, rapid or irregular heartbeat, sweating, and anxiety. This condition may require thyroidectomy. In that case, surgeons avoid posterior and inferior portions of the thyroid gland to preserve the parathyroid glands and not risk recurrent laryngeal nerve destruction.
Graves’ disease is an autoimmune disorder causing overproduction of T4 hormone. In this case, ophthalmopathy causes eyes to protrude from orbits due to tissue swelling within the orbit, leading to dry, red, irritated eyes with pressure in orbits. Dermopathy involves red, thickened skin on shins and the dorsum of feet.
Hypothyroidism is an underactive thyroid which causes fatigue, slow metabolism, obesity, sensitivity to cold, feeling sluggish, constipated, and heavy menstruation. This disease is caused by an autoimmune response (Hashimoto’s), radiation treatment, thyroid surgery, medications, a pituitary gland issue, or iodine deficiency.
Summary of anterior triangle and root of the neck
Whew! What a ride! From the boundaries and subtriangles, fascia, bones and cartilage, a joint, and large vessels supplying and draining blood from the head and neck, including lymphatic return to the venous system, several glands, to the many nerves coursing through this important region, we've covered quite a bit of ground in the anterior triangle and root of the neck. This is a high-yield, high-value, clinically relevant region to understand.
To complete the anterior neck, check out the post on the Lateral cervical region (posterior triangle) of the neck. And, use the contact page to send questions if you have them. Thanks for visiting AnatomyLove!