Lateral cervical region
The lateral cervical region (also known as the posterior triangle of the neck) contains important structures that connect the head and visceral neck to the arm and thorax. Several layers of fascia surround and define the triangle. Muscles related to this triangle are responsible for neck flexion, head rotation, head extension, and movements about the shoulder girdle. Many terminal portions of neurovascular bundles cross through it on their way to/from more distal targets of the neck and shoulder muscles and skin. Lymphatic drainage returns to the venous system in this area.
Context and overview of the lateral neck
The lateral cervical region - also known as the posterior triangle of the neck - contains important structures that connect the head and visceral neck to the arm and thorax. Several layers of important fascias surround and define the triangle. Muscles related to this triangle are responsible for neck flexion, head rotation, head extension, and movements about the shoulder girdle. Many terminal portions of neurovascular bundles cross through it on their way to/from more distal targets of the neck and shoulder muscles and skin. Lymphatic drainage returns to the venous system in this area.
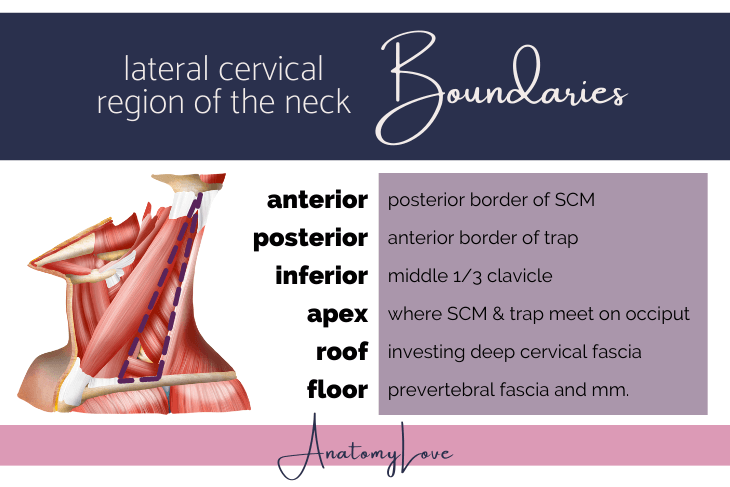
Boundaries of the lateral cervical region
First things first, let's figure out exactly what is meant by the "lateral cervical region" or posterior triangle of the neck.
The boundaries of this region are:
Anterior: posterior border of the SCM
Posterior: anterior border of trapezius m.
Inferior: middle 1/3 of the clavicle
Apex: where SCM and trap meet at the superior nuchal line
Roof: investing layer of deep cervical fascia
Floor: muscles covered by prevertebral layer of deep cervical fascia (splenius capitis m., levator scapulae m., anterior scalene m. (sometimes), middle scalene m., posterior scalene m.)
Based on the borders we see that the lateral cervical region (posterior triangle of the neck) lies between the two big neck muscles: SCM and trapezius, and right above the clavicle.
Now, anatomists are rarely satisfied with a simple triangle so this region is also subdivided in one large occipital subtriangle (superiorly) and one small supraclavicular subtriangle (inferiorly). The subtriangles are defined by their position relative to the inferior belly of the omohyoid m.
The occipital subtriangle is named for the occipital a. that courses through the superior portion of this sub-triangle.
The subclavian subtriangle (also known as omoclavicular or supraclavicular subtriangle) creates a palpable hollow above the clavicle (the greater supraclavicular fossa). The third portion of the subclavian a. courses through this area.
Contents of lateral cervical region
The contents of the lateral cervical region impact the head, anterior neck, shoulder, and the arm. Let's review them:
Scalene mm. and cervical portions of deep back muscles
Erb’s point (nerve point of the neck) and cutaneous cervical branches; CN 11 the spinal accessory n.; brachial plexus trunks
Subclavian vessels and branches/tributaries (cervicodorsal/transverse cervical a., suprascapular a.)
Portions of the external jugular v., carrying blood from the lateral scalp and face towards the subclavian v.
Supraclavicular lymph nodes
Muscular anatomy of the lateral cervical region
There are several palpable and visible features of the neck, especially in the lateral cervical region just above the clavicle. The sternocleidomastoid and trapezius muscles are boundaries of this triangle and their borders are easily seen and felt. The external jugular vein can also be seen in this region. Lymph nodes can be palpated in this region, just above the clavicle, too.
Platysma m.
From superficial to deep, let's start with a unique subcutaneous muscle, the platysma m. I think this muscle is cool because this thin muscle is really a muscle of facial expression but it is embedded within the superficial fascia of anterolateral neck.
The left and right platysma muscles occupy the superficial fascia and adipose of the anterolateral neck (it is absent anteriorly). It originates over the clavicles and pectoralis major m. and inserts over the inferior border of the mandible, blending with superficial chin muscles as high as the corners of the mouth.
The platysma is derived from the 2nd pharyngeal arch so it's innervation is SVE (special visceral efferent) fibers from the cervical br. of the facial n. The action is to tense the skin of the neck (“platysma face”) and pull down on the corners of the mouth.
Blood supply comes from the submental br. of the facial a., and suprascapular a.
Cutaneous branches of the cervical plexus pierce the platysma m. to reach the skin.
Sternocleidomastoid muscle
Sternocleidomastoid is a nice muscular landmark in the neck because it separates anterior and posterior (lateral cervical region) triangles of the neck. It is completely surrounded on anterior and posterior sides by lamina of the investing layer of deep cervical fascia. Let's review basic facts of the SCM before going on:
Note that the SCM has two heads, creating a lesser supraclavicular fossa between them. The two origins converge to insert together onto the lateral aspect of the mastoid process of the temporal bone and the lateral half of the superior nuchal line of the occiput.
This muscle is pretty wide, meaning that anterior and posterior bands of muscle fibers help this muscle produce different and sometimes counterintuitive actions. Unilaterally, one SCM produces lateral neck flexion and rotates the face toward the contralateral side. Acting together, bilaterally, anterior longitudinal fibers of the SCM flex the neck to bring the chin close to the chest. The posterior longitudinal fibers of this muscle are capable of extending the atlanto-occipital joint. When the cervical vertebrae are fixed these muscles help to expand the rib cage, acting as accessory muscles of respiration in times of duress.
Innervation to the SCM comes from the spinal accessory n., cranial nerve 11. Those motor fibers course through the superior aspect of the occipital subtriangle of this region because they also innervate the trapezius m. Pain and proprioception fibers from the SCM travel in cervical spinal nerves C2 and C3 VPR (ventral primary rami).
Blood supply to this large muscle comes from the occipital a. (a branch of the ECA or external carotid artery).
Trapezius muscle
The trapezius muscle is a large muscle that belongs to a discussion of back muscles. However, since the anterior border of the trapezius forms the posterior boundary of the lateral cervical region of the neck, we need to quickly review it here. Note that like the SCM, the trapezius is wrapped by lamina of the investing layer of deep cervical fascia.
The trapezius originates on the skull and vertebral column (medial 1/3 of superior nuchal line, EOP, nuchal ligament and spinous processes from C7-T12) and inserts on the pectoral girdle (lateral 1/3 of the clavicle, acromion, and spine of scapula).
Contraction of the trapezius m. acts on the scapula and head. It is capable of elevating the scapula through descending fibers, depressing the scapula through ascending fibers, retracting the scapula through transverse fibers, scapular rotation (glenoid cavity moves superiorly as the arm abducts) via descending/ascending fibers, extending the head when acting bilaterally and shoulders are fixed, and finally, laterally flexing the head towards the ipsilateral side when acting unilaterally.
The nerve that provides motor innervation to the trapezius m. is the spinal accessory n., cranial nerve 11. Test this muscle by asking patient to shrug shoulders against resistance (normal if muscle borders are easily seen). Pain and proprioception fibers from the VPR (ventral primary rami) of C3 & C4 also supply the trapezius m.
Blood supply comes from the superficial br. of transverse cervical (cervicodorsal), occipital, and dorsal scapular aa.
Scalene muscles
The scalene muscles - anterior, middle, and posterior - form the majority of the floor of the lateral cervical region. The scalene muscle group helps in understanding anatomical relationships in the neck broadly. They are wrapped in prevertebral deep cervical fascia.
The anterior scalene m. especially is a good landmark:
The phrenic nerve and ascending cervical a. course along the anterior surface of anterior scalene m.
The subclavian vein passes anterior to the anterior scalene while the subclavian artery passes deep to it.
The roots of the brachial plexus emerge from between the anterior and middle scalene muscles.
Let's review the scalene muscles as a group:
All three of the scalene muscles originate from transverse processes of cervical vertebrae and insert on the ribs.
The mnemonic I use to keep the origins straight is: 36-27-46 APP or “hourglass scalenes”
The digits refer to transverse processes of origin for anterior-middle-posterior scalene mm. and the APP refers to the tubercles of the transverse process (anterior-posterior-posterior).
Using the mnemonic we see that the anterior scalene m. uses the anterior tubercle of the transverse process at the C3-6 levels. Middle scalene m. uses the posterior tubercle of the transverse process at C2-7 levels. Finally, the posterior scalene originates from the posterior tubercles of transverse processes of C4-6 cervical vertebrae.
Insertions of the scalene muscles are straight-forward by comparison. The anterior scalene m. has a dedicated tubercle on the superior aspect of rib 1. Two big grooves lie on either side of it - the groove for subclavian vein anteriorly and groove for subclavian artery posteriorly. The middle scalene m. also inserts onto the superior aspect of rib 1, though it is just a rough area, not a whole tubercle. The posterior scalene m. inserts on rib 2.
Blood vessels that supply the shoulder course anterior to the anterior scalene m. - these are transverse cervical a. (also known as cervicodorsal trunk) and the suprascapular a. These two come from the thyrocervical trunk, the third branch from the first part of the subclavian artery. A small ascending cervical a. (itself a branch of inf. thyroid a., also from the thyrocervical trunk) courses on the anterior aspect of the anterior scalene m. - along with the phrenic n. I told you the anterior scalene m. is a great landmark in the neck!
Importantly, roots of the brachial plexus emerge from between the anterior and middle scalene mm. to course through the supraclavicular/subclavian/omoclavicular subtriangle. They can become pinched between these muscles and/or between them and the clavicle as they pass into the axilla.
Another relationship of note, regarding the middle scalene m., is that the dorsal scapular and long thoracic nn., both from proximal parts of the brachial plexus, pierce the middle scalene m. and emerge from it’s lateral side. Since these nerves provide motor innervation to mid-back muscles (levator scapulae, rhomboid major, rhomboid minor mm. from the dorsal scapular n.) and the serratus anterior m. (from the long thoracic n.), these muscles are affected should the middle scalene m. become hypertrophied or spasm.
Vessels of the lateral cervical region
In this region we need to review the subclavian vessels since they and their branches supply this triangle and course through it to other targets in the deep neck and shoulder.
Subclavian artery
In this region we need to review the subclavian vessels since they and their branches supply this triangle and course through it to other targets in the deep neck and shoulder.
First let's remember that there is asymmetry of the subclavian arteries: the L side is direct branch of the aortic arch while the R side is a branch of the brachiocephalic trunk (itself a branch of the aortic arch). Both sides course through the root of the neck and into the lateral cervical region.
The subclavian arteries pass deep to the anterior scalene m. (leaving a large groove on the superior aspect of rib 1). The subclavian veins pass superficial to the anterior scalene m. (and also leave a large groove on the superior aspect of rib 1 at that location).
Three portions of the subclavian a. are defined by their position relative to the anterior scalene m. (it is a great landmark in the neck!).
Part 1 - medial to anterior scalene m. - gives rise to the vertebral a., internal thoracic a., and thyrocervical trunk
Part 2 - posterior to anterior scalene m. - gives rise to the costocervical trunk
Part 3 - lateral to anterior scalene m. - may or may not give rise to the dorsal scapular a.
Subclavian vein
The subclavian veins pass through the lateral cervical region, having come from the axilla and arm - they are the medial continuation of the axillary vein, which changes its name to subclavian as it passes by the lateral border of rib 1. As the subclavian v. courses medially it passes superficial to the anterior scalene m., leaving a groove on rib 1 as it continues between it and the clavicle.
Where the subclavian v. meets the IJV (internal jugular vein) they form the venous angle. Lymphatics empty into the venous angles (right lymphatic duct, thoracic duct on left side).
To get venous blood back into the heart, the brachiocephalic veins form medial to the venous angles. The two brachiocephalic veins meet to form the superior vena cava which empties straight into the right atrium.
Lymphatic drainage in the neck
Lymphatic fluid of the face and lateral scalp drains into the neck.
Superficial cervical lymph nodes are scattered along the EJV (external jugular vein). These drain into deep cervical lymph nodes along the IJV (internal jugular vein).
Lymphatic vessels return lymph to the venous system at the venous angles, the junction of the subclavian v. and IJV. On the left side they form the thoracic duct and on the right side they form the right lymphatic duct.
Nerves of the lateral cervical region
One of the hallmarks of dissecting this region is the messy tangle of nerves and vessels coursing through the lateral cervical region. Here we'll find a cranial nerve as well as portions of the cervical and brachial plexuses of nerves. Nervous innervation to the neck, shoulder, and arm all move through this triangle and it is a wild ride, so let's get going!
Spinal accessory n., cranial nerve 11
A prominent nerve of the occipital subtriangle of the lateral cervical region is the spinal accessory n., cranial nerve 11. It exits the jugular foramen of the skull then heads towards the sternocleidomastoid and trapezius muscles to provide motor innervation to them. It is large and quite wavy here, making it easier to pick out among the rest of the nerve tangle. And, it is a bit superficial, being related to the investing layer of deep cervical fascia.
Cervical plexus and Erb's point, or the nerve point of the neck
The cervical plexus consists of the VPR (ventral primary rami) of spinal nerves C1-C4. Loops connect the VPR, making dissection extra fun! The cervical plexus has a lot of branches - motor, sensory, and both types of fibers. In the lateral cervical region we're dealing with the cutaneous sensory branches that emerge at Erb’s point (nerve point of the neck) and a few branches to the trapezius and sternocleidomastoid mm.
The portions of the cervical plexus that course through the lateral cervical region include those C2-3 VPR providing pain and proprioception to the SCM and some from C3-4 VPR doing the same for the trapezius.
Then, four sensory cutaneous branches course from the nerve point of the neck (also known as Erb's point), located along the posterior border of the SCM, just above the half-way point.
Lesser occipital n. forms from C2 and courses towards scalp behind the ear
Great auricular n. comes from C2 & 3 and courses up towards the angle of the mandible and parotid region, providing the only cutaneous sensory innervation to the face that does not come from the trigeminal n. (CN 5)
Transverse cervical n. also forms from C2 & 3 and it crosses anterior to the SCM in a transverse fashion (thus the name) to reach skin of the anterior triangle of the neck
Supraclavicular nn., forming from C3 & 4 and grouping up into medial, intermediate, and lateral clusters, provide sensory innervation over the clavicle and upper aspects of the pectoral region.
There are more branches of the cervical plexus but they move anterior into the anterior triangle of the neck to provide motor innervation there by way of the ansa cervicalis n. We'll cover them later!
Brachial plexus roots and trunks
The whole brachial plexus is formed from the VPR (ventral primary rami) of C5-C8 and T1. The roots emerge from between the anterior and middle scalene mm. and can be dissected in the lateral cervical region. Those roots form 3 trunks and 2 divisions within the omoclavicular sub-triangle and deep to the clavicle. The brachial plexus then enters the cervico-axillary canal between rib 1 and the clavicle, running inside the axillary sheath, an extension of the prevertebral fascia.
Though the large roots themselves lie between anterior and middle scalene mm. in the lateral cervical region, as mentioned above, two branches of the roots of the brachial plexus actually pierce the middle scalene m. to get to their targets. The dorsal scapular n. from the C5 root, and the long thoracic n. from C5-C7 can both be found coming out of the lateral side of the middle scalene m. The dorsal scapular n. innervates the levator scapulae, rhomboid major, and rhomboid minor mm. of the mid-back. The long thoracic n. innervates the serratus anterior m.
Whoa! There is a lot going on in this little triangle in the lateral cervical region of the neck. I hope you found this review of the muscles, vessels, and nerves of this region useful! Scroll up and download one of my drawings of the vessels if you need it. Or scroll down to see additional posts!