Superficial face and parotid region
The human face contributes greatly to our identity and capacity for non-verbal communication. The muscles that express our internal state of being are called muscles of facial expression. They share innervation (facial n.), a large portion of blood supply (facial a.). Sensation on the face is the job of the trigeminal n. This, coupled with the presence of a large salivary gland, the parotid, make the face a useful diagnostic tool for any clinician.
The human face contributes greatly to our identity and capacity for non-verbal communication. The muscles that express our internal state of being are called muscles of facial expression. They share innervation (facial n.), a large portion of blood supply (facial a.). Sensation on the face is the job of the trigeminal n. The largest salivary gland, the parotid gland, is also part of the superficial face region. The face is a useful diagnostic tool for any clinician.
Click through and read what you need, and/or scroll to the bottom for a
downloadable drawing and key for everything superficial face!
Surface features of the face
Because by definition the superficial face is highly visible, it is important to review external features that can be inspected and may have clinical relationships to the neurovascular and muscular structures within the face and cranial cavity.
The external features related to the orbit include:
Palpebrae - a fancy anatomical word for "eye lids," meaning there are both superior (upper) and inferior (lower) palpebrae
Palpebral fissure - another fancy anatomical word that refers to the opening between palpebrae/eye lids; don't take this for granted because an inability to fully close the palpebral fissure leaves a dry and irritated eye and conjunctiva lining and may be indicative of nervous or muscular problems in the structures that open and close the palpebrae
Medial and lateral canthi - think "corners" of the eyes, one towards the nose (medial) and one towards the temple (lateral); because these are both anchored to the surrounding bony orbit they should be level with one another when the head is in proper anatomical position; the medial canthus contains several structures important in lacrimation and the drainage of tear fluids from the eye
Like the eye and orbit, external features related to the nose are clinically relevant since they protect and allow inspection of the nasal cavity. These structures include:
Dorsum of the nose - the long part of the nose that runs from the bridge between the eyes to the tip of the nose
Ala of the nose - coverings of skin and connective tissues that surround the nostrils; these are what fan out when you "flare" your nostrils at someone
Anterior nares - a fancy anatomical words for the opening of the nostrils (or like I call them, "anterior nose holes!")
Nasolabial fold - like the name implies, this is a crease that runs from the alae of the nose to the corners (commissures) of the mouth
Philtrum - that little divot right under the nose, connecting the nasal septum to the upper lip (sometimes lovingly referred to as the "snot catcher")
The mouth is the entrance to the oral cavity and therefore both the respiratory and gastrointestinal systems. Visual inspection of this area is just as clinically relevant and informative as the rest of the facial regions. External features related to the mouth include:
Oral fissure - the opening between upper and lower lips
Vermillion border - a transition point between the "outside" of the lips (like skin) and the "inside" of the lips (a mucous membrane)
Labial commissure - corners of the mouth (because anatomists are apparently unable to just call them that!)
Mental protuberance - the point of your chinny chin chin, right in the midline
Scalp
The scalp is the skin and connective tissues that cover the cranium. Though continuous with the rest of the skin, of course, the scalp itself runs from the supraorbital margins of the orbits to the superior nuchal line on the occiput and from zygomatic arch to zygomatic arch.
The scalp is organized into 5 layers that conveniently enough spell the acronym S-C-A-L-P:
Skin
Connective tissue
Aponeurosis (musculotendinous)
Loose areolar tissue
Pericranium
One note about those layers, and something that is a bit puzzling to me, though if we think about it too hard the SCALP mnemonic doesn't work...but let’s talk it out!
"Skin" is technically epidermis (epithelial tissue) plus the dermis (dense irregular connective tissue). In the SCALP mnemonic, I interpret the first layer (Scalp) or "skin," as just the epidermis and the second layer (sCalp) or "connective tissue," as the dermal layer. My reasoning here is that the first three layers of scalp, the skin and connective tissue plus the tough aponeurosis (scAlp), glide as a unit on the fourth layer (scaLp) which is a thin layer of loose areolar connective tissue. When we do things like raise our eyebrows we can feel those top three layers slide around.
The aponeurosis is musculotendinous, meaning it contains a little of both those tissues. Embedded in the anterior aspect of the cranial aponeurosis is the frontalis muscle (the one the wrinkles skin on the forehead and elevates the eyebrows). The posterior aspect of that same aponeurosis includes the occipitalis muscle, pulling the scalp skin down towards the neck, or retract the scalp. These two muscle bellies at opposite ends of the aponeurosis is one reason scalp wounds gape and split so readily (and bleed profusely in the process). The muscles pull on the sheet of connective tissue, leaving it open and allowing view of the underlying cranial bones.
Speaking of the deepest layer (scalP) and the bones it covers...the pericranium is synonymous with the periosteum of the ectocranial surface of the cranial bones. It is adhered to the bones and especially to the sutures between them, and therefore immobile.
Parotid gland
The parotid gland is named for the location - par (near) the otid (ear). As a salivary gland it must deposit saliva into the mouth and we'll discuss that below, but first we need to get solid on the position of this gland and why it must be included with a discussion of the superficial face.
Position of the parotid gland
We know the parotid gland lies just in front of the ear, as it's name implies. However, what many students don't expect is how just darn big and extensive the parotid gland can be! It is the largest salivary gland, in fact!
Most of this gland lies external (superficial) to the ramus of the mandible, which by definition puts it in the superficial face (as opposed to the deep face and infratemporal fossa of the head, deep to the mandible). Often, parts of the gland will wrap around the ramus of the mandible, forming a deep portion of the gland there.
The superficial nature of this gland mean that it is contained within the parotid sheath/capsule derived from the investing layer of deep cervical fascia. This is tough, fibrous fascia that limits expansion of the gland and compresses related structures instead (more on that below).
The parotid can extend from the zygomatic arches all the way down into the neck and sometimes below the angle and inferior border of the mandible. Anteriorly it usually extends beyond the ramus of the mandible, more into the "cheek" region, proper. It is about half the size of your palm, in other words.
Parotid duct
The parotid gland has one large duct called the parotid duct (sometimes still referred to as Stenson's duct). The duct courses from the anterior border of the gland, transversely across the cheek just under the zygomatic arch, then dives into the mouth by piercing the buccinator muscle (technically a muscle of facial expression we'll discuss below). The parotid duct opens into the mouth at the parotid papilla, located in the upper cheek near the second maxillary molar. You can feel yours with your tongue, I bet! Accessory parotid glandular tissue often extends down the length of the duct, too.
Parotid gland histology
The parotid salivary gland produces entirely serous secretions and no mucous secretions, unlike the other salivary glands that produce mixes of both (this is quite evident in histological images of the parotid gland). It looks just like the pancreas except it does not have islets of the Langerhans (the endocrine portion of the pancreas).
This exocrine salivary gland is formed by simple cuboidal epithelial cells organized into acini (like cul-de-sacs of simple cuboidal cells). The entirely serous secretions (proteinaceous and watery) flow into intercalated ducts of low cuboidal epithelium which then join into striated then interlobular ducts.
Innervation to the parotid gland
Salivary glands require parasympathetic secretomotor innervation (GVE general visceral efferent fibers) to produce their products. There are only 4 parasympathetic cranial nerves (3, 7, 9, and 10) so that really limits our options for glands in the head. Since cranial nerve 3's parasympathetic targets are in the orbit and 10's are largely below the neck, that leaves the facial nerve (7) and the glossopharyngeal nerve (9). All glands EXCEPT the parotid gland are innervated by the facial nerve so that means...glossopharyngeal nerve is left to innervate the parotid gland.
The trip these nerves take to the parotid gland is wild, as is typically the case with parasympathetic innervations in the head.
The pre-ganglionic neurons for the parotid gland lie in the inferior salivatory nucleus of the medulla. Like the rest of the glossopharyngeal nerve fibers, they exit the cranial cavity through the jugular foramen. But! These need to get back into the head so the pre-ganglionic fibers use the tympanic canaliculus to re-enter the petrous portion of the temporal bone. In the middle ear they form the tympanic plexus then emerge from the anterior aspect of the petrous portion of the temporal bone into the middle cranial fossa as the lesser petrosal nerve. This nerve puts a groove in the floor of the middle cranial fossa headed from the petrous temporal to the foramen ovale.
The lesser petrosal nerve exits the skull through foramen ovale (along with the mandibular division of the trigeminal nerve). Why? Because the otic ganglion, the location of the post-ganglionic neurons that belong to this pathway, are literally dangling off of the mandibular division of the trigeminal nerve. This type of relationship between branches of the trigeminal nerve and parasympathetic fibers occurs often in the head. The pre-ganglionic fibers in the lesser petrosal nerve synapse in the otic ganglion. From there, post-ganglionic axons hitchhike with the auriculotemporal nerve, a sensory branch of the trigeminal nerve that innervates skin and adjacent structures just in front of the ear. This offers the parasympathetic fibers from the glossopharyngeal nerve a convenient route to get to the parotid gland in that region. Viola! Now saliva can flow from the parotid gland!
There are sympathetic fibers at play too, but their target is the vessels that supply the gland, not the gland itself. Vasomotor sympathetic innervation of these vessels reduces blood flow (and thereby the raw product out of which saliva is made).
Sensory innervation of the parotid gland travels in trigeminal's auriculotemporal nerve and in the great auricular nerve, a sensory branch from C2-3 ventral primary rami (VPR) of the cervical plexus.
Important relationships of the parotid gland on the superficial face
Besides the position of the parotid gland placing it squarely within superficial face territory, another reason to cover it here has to do with the structures that are related to the gland.
The facial nerve literally runs right through the middle of the parotid gland. Why is this important? The facial nerve does NOT innervate the parotid gland itself (remember that is done by the glossopharyngeal nerve). However, these facial nerve branches are the ones that provide motor innervation to the muscles of facial expression - the ones that lie just deep to the skin and cause it to move around! We'll cover those in detail elsewhere on this page, and I'll remind you of the relationship between the facial nerve and the parotid gland.
Two large vessels are related to the parotid gland, too. The retromandibular vein and the external carotid artery run within the deeper aspects of the gland, just behind the ramus of the mandible. These are both big vessels! Retromandibular vein drains blood from the deep face and lateral aspects of the scalp while the external carotid artery branches distal to this location (maxillary and superficial temporal arteries) supply the same regions with blood.
Clinical complications of the parotid gland
Parotid tumors may develop in the parotid gland, especially since it is the biggest of such glands. Most are benign, though salivary gland cancers are likely to form in the parotid rather than other glands, given it's size.
If required, parotidectomies endanger the motor fibers in the facial nerve (the ones to muscles of facial expression). Surgeons use imaging to avoid damaging those motor fibers because that would paralyze the muscles they innervate.
Infection and abscesses of the parotid gland may also occur, especially due to the mumps virus. Inflammation of the parotid gland looks like a swollen face and cheek, typically on one side only. It is accompanied by severe pain because the parotid sheath is so tough. Pain may be exacerbated by opening the mouth, as the gland would be pushed into the mastoid process posteriorly. Inflammation of the duct or parotid papilla is also possible. Bacterial infections produce pus and an abscess, producing pain from the swelling.
Blockage of the parotid duct may occur from calcifications (sialoliths/pebbles) of saliva. These cause pain along the parotid duct and the pain is made worse by eating since the secretions are blocked within the duct.
Muscles of facial expression
Muscles of facial expression do just that - they express emotions and your internal state of being by moving the skin of the face - how cool is that?!
These muscles originate from bone and insert onto subcutaneous tissue and skin - that is how they move the skin itself.
This group is derived from mesoderm of the second pharyngeal arch of an embryo, meaning their nerve is the facial nerve since that is what innervates all muscles from that arch.
Note: the masseter muscle is a muscle of mastication (not facial expression) but it is easily seen with
superficial face dissections.
It is useful to subdivide muscles of facial expression into regions of the face. These muscles will be named for their position (frontalis, for example), and/or their action (levator labii superioris just has to elevate the upper lip!). Pay attention to the names for the reason that they will tell you their insertion sometimes, too - labii to the lips, anguli to the angle of the mouth, etc. Ok, let's go!
Muscles related to the frontal and orbital region:
frontalis m. (anterior belly of occipito-frontalis m.) - elevates the eyebrows and wrinkles skin on the forehead
orbicularis oculi m. (palpebral and orbital parts) - closes the upper eyelid (palpebrae) and squeezes it shut
procerus m. - eyebrow muscle that wrinkles the skin of the medial brow
corrugator supercilii m. - eyebrow muscle that scrunches up the medial brows, drawing them down and in
Muscles related to the midface, nose, and upper lip include:
nasalis m. - not well developed in humans but this muscle can help flare the nostrils
zygomaticus minor m. - elevates and retracts the upper lip
zygomaticus major m. - elevates and retracts the corner of the mouth (labial commissure)
levator labii superioris m. - elevates the upper lip
levator labii superioris alaeque nasi m. - elevates the upper lip and helps flare the nostrils
levator anguli oris m. - elevates the corner of the mouth (labial commissure)
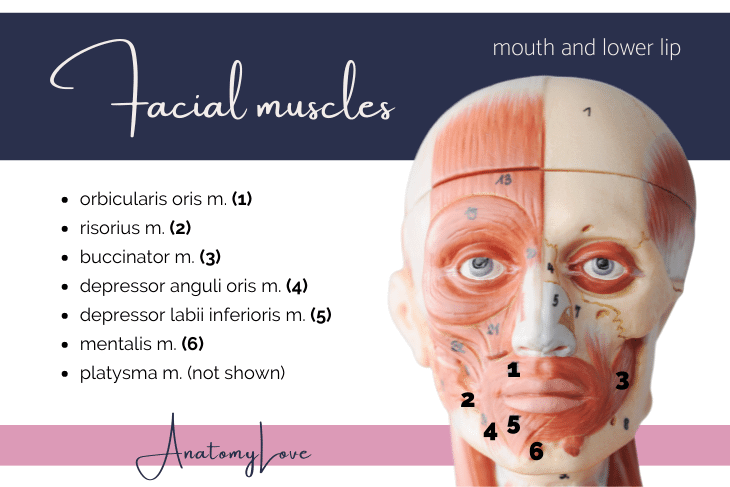
Muscles related to the mouth and lower lip include:
orbicularis oris m. - circles and helps close the mouth
risorius m. - retracts the corners of the mouth (labial commissure)
buccinator m. - cheek muscle that pushes food against the teeth while chewing
depressor anguli oris m. - pulls down on the corner of the mouth (labial commissure)
depressor labii inferioris m. - pulls down on the lower lip
mentalis m. - wrinkles the skin on the chin
platysma m. - superficial muscle of the neck that tightens the skin of the neck and pulls down on the corners of the mouth (see posts on the lateral cervical region or posterior triangle of the neck for more info on platysma muscle)
Facial nerve and motor innervation to facial muscles
Isn't it beautiful that the nerve that provides muscles of facial expression is named the facial nerve?! I mean, what else would it be called, after all? The facial nerve does so much on the face, from parasympathetic innervation to most salivary and mucosal glands to tasting from the anterior two-thirds of the tongue to innervating the smallest muscle in the body, the stapedius (it dampens vibrations on the tympanic membrane of the ear so things aren't too loud)...and it innervates many muscles on the face, too - wowza!
The facial nerve is cranial nerve 7. It's nuclei lie in the pons and it's fibers exit the cranial cavity at the internal auditory meatus. The intermediate nerve contains the sensory and parasympathetic roots of the facial nerve. Chorda tympani nerve carries those sympathetics and the special sensory fibers from the tongue.
Inside the petrous portion of the temporal bone the facial nerve divides into a few key branches. The fibers we need for muscles of the face exit the petrous temporal bone at the stylomastoid foramen, located just under and behind the ear lobe.
This portion of the facial nerve consists of SVE (special visceral efferent) fibers that specifically innervate skeletal muscle derived from the second pharyngeal arch of a developing embryo. For more on the types of fibers in cranial nerves, see the post on Introduction to Cranial Nerves.
Full disclosure, the facial nerve contains just a few sensory fibers that overlap with branches of the vagus nerve to innervate the auricle and conchae of the external ear. But, because that is rather small and insignificant (and overlapped by vagus nerve), we won't go in to depth with them here.
The motor fibers that exit at the stylomastoid foramen innervate:
small auricular muscles embedded in the scalp around the ear
the stapedius muscle inside the ear
posterior digastric and stylohyoid muscles of the anterior triangle of the neck
all muscles of facial expression
Most muscles on the face are innervated by more than one branch of the facial nerve, and there are five terminal branches to make sure everyone gets covered:
Temporal br. - courses superiorly towards the "temple" region, innervating muscles like orbicularis oculi and frontalis
Zygomatic br. - a few branches form right along the zygomatic arch and supply the orbicularis oculi muscle, the zygomaticus major and minor muscles, elevators of the lip, and dilators of the nostrils
Buccal brs. - there are typically 2-3 of these coursing transversely across the cheek, usually parallel to the parotid duct; they innervate the two zygomaticus muscles, buccinator muscle, risorius, and the elevators of the lip
Marginal mandibular br. - this one rides near the inferior border of the mandible and innervates muscles on the chin and depressors of the lower lip
Cervical br. - named because it courses inferiorly towards the platysma muscle, the cervical branch of the facial nerve innervates just that superficial muscle of the neck
Clinical aspects of facial nerve
Naturally, assessing the facial nerve is clinically important and can be done in quite a number of ways given the distribution and variety of innervations this nerve contains.
First, a peculiar fact about the facial nerve and it's innervation of muscles that act in unison on right and left sides of the body (a full and balance smile, not a smirk, or raising both eyebrows instead of one, for example). Normally, motor neurons that innervate muscles that act in unison (muscles for mastication, deglutition, phonation, and movements of the tongue) are influenced by corticobulbar tract fibers in both cerebral hemispheres. Facial muscles are the exception to that rule.
Upper facial muscles receive bilateral (ipsi- & contralateral) cortical inputs
Middle and lower facial muscles only receive unilateral (contralateral only) cortical inputs
A lesion of an upper motor neuron will only affect the contralateral lower facial muscles because the upper facial muscles receive inputs from both left and right motor cortices.
However, a lower motor neuron lesion (one that impacts muscles of the contralateral upper AND lower facial muscles), shows up as paralysis all facial muscles on one side.
Another cause of paralysis of facial muscles is known as Bell’spalsy. Technically this is a lesion of the lower motor neuron fibers that affects all facial muscles (upper and lower) on one side. Bell's palsy can result from compression of the nerve or a virus and/or inflammation around the stylomastoid foramen and facial nerve as it runs through the parotid gland. Bell's palsy leaves the eye dry and irritated due to the loss of the ability to blink, sometimes leading to corneal ulcerations. Loss of innervation to the stapedius muscle allows more vibration at the tympanic membrane (allowing noise to reverberate and be loud). Additionally, loss of taste from the anterior two-thirds of the tongue may happen if the inflammation affects the chorda tympani nerve.
Trigeminal nerve and sensation from the face
With so much talk of the facial nerve and it's motor innervation to muscles of facial expression, we cannot forget FEELING or sensations from the face which are served by the trigeminal nerve, cranial nerve five.
To reach all areas of the face, the trigeminal nerve is broken up into three large divisions (hence the name, TRIgeminal nerve). The trigeminal nerve is the nerve to structures derived from mesoderm in the first pharyngeal arch of a developing embryo.
Each division of the trigeminal nerve serves a dermatome of the face, roughly divided into upper face, midface, and lower face. Because roman numerals are often used to discuss cranial nerves, you might see these nerves abbreviated as V1, V2, and V3 for the ophthalmic division, maxillary division, and mandibular division of the trigeminal nerve, respectively.
Importantly, this cranial nerve contains both motor and sensory fibers but not in all divisions. The ophthalmic division (V1) and maxillary divisions (V2) are all sensory. Not a motor fiber can be found in these nerves! However, the mandibular division (V3) contains both motor and sensory fibers. The motor fibers in V3 run the muscles of mastication (temporalis, masseter, lateral pterygoid, medial pterygoid, a few small muscles beneath the chin) so they will not be discussed here since they are part of the "deep face" or infratemporal fossa.
Key landmarks for defining the dermatomes on the face are the lateral canthi of the eyes and the lateral commissures of the mouth. And, it is important to notice that the dermatomes do not just go straight back from there - they curve up, like a smile.
Course
Each division of the trigeminal nerve provides general somatic afferent/sensory (GSA) innervation from the face, meaning it provides the feelings of touch, pain, and temperature sensations.
The ophthalmic division (V1) has five terminal branches that spread out over the forehead, eyebrow, upper eyelid, and down the dorsum of the nose. All branches of V1 move through the orbit to reach the face (V1 exits the cranial cavity at the superior orbital fissure, a large opening between the greater and lesser wings of the sphenoid bone located at the back of the orbit. The terminal branches of V1 are: lacrimal, supraorbital, supratrochlear, infratrochlear, and external nasal nerves. The largest V1 branch are the pair of supraorbital nerves (medial and lateral) that reach the face by coursing through the supraorbital notch (sometimes it is a foramen instead) located along the superior margin of the orbit.
The maxillary division (V2) has three branches to the superficial face. The largest and most expansive is the infraorbital nerve that reaches the face via the infraorbital foramen of the maxilla. Two other small nerves complete this dermatome on the cheek - zygomaticofacial and zygomaticotemporal (they exit via foramina of the same name on the zygomatic bone).
The mandibular division (V3) is the largest portion of the trigeminal nerve because it contains sensory fibers that we're about to review here, as well as motor fibers to muscles of mastication (temporalis, masseter, lateral pterygoid, medial pterygoid, small muscles under the chin) that will be reviewed in a separate post. All parts of the mandibular division of trigeminal exit the cranial cavity at foramen ovale - a large opening in the greater wing of the sphenoid bone on the base of the cranium. Terminal sensory branches to the superficial face from V3 are: mental, buccal, and auriculotemporal nerves. The largest of those is the mental nerve which pops out of the mandible through a foramen of the same name. Buccal means "cheek" so this nerve heads straight there from the foramen ovale. The auriculotemporal nerve exits from foramen ovale and heads laterally towards the temporomandibular joint (TMJ) to reach the area immediately in front of the ear. If you read about the parotid gland above, you know that the auriculotemporal nerve carries the secretomotor fibers to the parotid gland as hitchhikers.
While it is useful to know all the terminal branches of the trigeminal nerve on the face, there are three that are especially important for clinical testing of the trigeminal nerve on the face. I call these the "cardinal" nerves of the trigeminal. And, they are all in a line, each within their own dermatome - V1, V2, and V3.
Because the dermatomes of the face are not straight-forward on the side of the head, testing of the trigeminal nerve should occur on the front of the face at the location of these "cardinal nerves" which are supraorbital, infraorbital, and mental. Notice they lie along the same line, parasagittal to the nose. Nice!
Arterial supply to the face and scalp
Like the facial nerve, it is nice that the primary artery to the superficial face is the facial artery, a large branch of the external carotid. Review the post on the anterior triangle of the neck to learn more about the external carotid artery.
The facial artery leaves the external carotid and heads superiorly. It actually dives behind the stylohyoid and posterior digastric muscles, as well as the submandibular gland. It gives off a submental artery to that subtriangle of the neck before coursing up and over the inferior border of the mandible to reach the superficial face.
Branches of the facial artery on the superficial face proper include:
Inferior labial artery to the lower lip and chin
Superior labial artery to the upper lip
Lateral nasal artery to the alae of the nose
Angular artery (the terminal branch of facial artery) towards the medial corner/canthus of the eye
One quick note about arterial supply to the scalp (because these are not facial artery branches):
Occipital artery (another branch of the external carotid) supplies the posterior aspect of scalp
Posterior auricular artery (also a branch of the external carotid) supplies scalp just behind ear
Superficial temporal artery supplies the face immediately in front of the ear and the lateral side of the face (the "temple")
Infraorbital artery (a branch of the maxillary, itself a branch of external carotid) supplies the midface
Supratrochlear and supraorbital arteries come from the ophthalmic artery, a branch of the internal carotid artery from the orbit
Venous return from the face and scalp
The quickest way to understand venous drainage of the superficial face is to look at the named arterial branches of the facial artery and reverse the blood flow because with one exception, venous return of the anterior face mirrors the facial artery branches.
Angular v. forms at medial canthi and connects to ophthalmic veins in the orbit and therefore with the cavernous sinus inside the cranial cavity, too
External nasal vein from the side of the nose
Superior labial vein from the upper lip
Deep facial vein from the cheek (notice this one wasn't mentioned in terms of arterial supply; it is a connection between the facial vein superficially and the pterygoid venous plexus in the deep face/infratemporal fossa)
Inferior labial vein from the lower lip and chin
The facial vein crosses the inferior border of the mandible posterior to the facial artery. It flows into the digastric/submandibular subtriangle of the neck where it meets the submental, lingual, and anterior division of the retromandibular veins to make a rather large common facial vein. Blood then empties into the internal jugular vein.
As for the arteries discussed above, portions of the lateral scalp are drained by the superficial temporal veins, retromandibular vein, posterior auricular vein, and the external jugular vein. Posterior scalp drains into occipital veins which usually form a venous plexus, but sometimes reach the internal jugular vein.
Summary of the superficial face and parotid region
Well, that's about it! Big topics in terms of the superficial face are: muscles of facial expression, their motor nerve the facial nerve, their blood supply from the facial vessels, and feeling from the face via the trigeminal nerve. The large parotid salivary gland comes into play because it is so prominent near the ear and technically part of the superficial face. I hope this review has been useful! If you'd like a drawing that puts all of this together, use the download button below!